Note: This is Part 2 of a two-part series on the Physical Degeneration of Man. Part 1 is here.
PDF: We created a clean, printable PDF of this post for offline reading. Buy it here or view a preview.
___________
If fiat currency has reshaped markets, built empires, and fueled wars, its impact on society goes far deeper than just economics. It has infiltrated every aspect of modern life, altering not just how we trade and govern but how we live, eat, and even think, creating negative externalities. It has now become econopathogenic.
In Part 1, we examined the historical and economic forces that shaped fiat currency’s transformative power. Now, in Part 2, we turn our focus to the fallout—a closer look at how this system has quietly eroded the very pillars of health, sustenance, and human vitality.
The question now is not what fiat has built, but rather:
What has it destroyed?
When President Nixon closed the gold window in 1971, he set in motion a chain reaction that would redefine not only economics but also the American food system.
Freed from the constraints of the gold standard, politicians quickly pivoted to incentivize mass production, industrialization, and monoculture farming.
These changes, while lowering food costs and increasing food production and distribution, came at a steep price: the degradation of our soil, our food, and, ultimately, our bodies.
Fiat Diseases
The policies we discussed in Part 1 have been extremely effective in shaping consumer choice in America, most notably, in deciding what foods we eat.
Between 1970 and 2014, Americans’ per capita consumption of several traditional foods significantly declined:
- Red meat: Down 28%
- Whole milk: Down 79%
- Eggs: Down 13%
- Animal fats: Down 27%
- Butter: Down 9%
In contrast, consumption of less healthy alternatives sharply rose:
- Toxic “vegetable” oils: Up 87%
- Grains: Up 28%
Americans showed exemplary compliance with government dietary guidelines, significantly increasing their consumption of fresh fruits and vegetables.



This data strongly suggests the root cause of rising obesity rates is not a lack of fruits and vegetables, but rather the decline in red meat consumption, which is a key source of essential nutrients.
Overall meat consumption remained stable, increasing by just 2%, but this came at a cost: highly nutritious red meat was replaced with cheaper, inferior, mass-produced poultry.
Author’s note: This shift is exemplified in Chick-fil-A’s marketing slogan, “Eat Mor Chikin,” which was first introduced in 1995 when two cows painted it on a billboard in Atlanta, Georgia.
As a result of all the big business propaganda, special interest and government influence, calories from animal foods dropped by 21%, while calories from plant-based foods rose by 14%.
So, that leaves us in somewhat of a conundrum.
Is junk food the main problem?
This is not clear.
Since 2001, Americans have cut back on sugar and refined carbs, while increasing whole grains:

Based on the data, it appears Americans have followed all of the government recommendations, but yet, American health has not improved.
Since 1980:
- Adult obesity rates have doubled; they are projected to increase another 50 percent by 2030.
- Two-thirds of U.S. adults are overweight, and one-third are obese.
- 25 million American adults have diabetes.
- Childhood obesity and diabetes diagnoses have tripled.
Epidemiological data show increases in incidence and prevalence of diseases associated with endocrine-disrupting chemicals, such as breast, prostate, and testis cancer, diabetes, obesity, and decreased fertility over the last 50 years.
A short overview of supporting data is presented below:

Data shows a consistent increase in the number and percentage of the U.S. population diagnosed with diabetes between 1958 and 2014. The percentage of the U.S. population with diabetes rose from 1% in 1958 to over 7% in 2014. Simultaneously, the absolute number of individuals with diabetes increased from less than 2 million in 1958 to over 20 million by 2014, reflecting both population growth and a rising prevalence of the disease. The sharpest rise in both metrics occurred after the late 1990s, signaling a significant acceleration in diabetes diagnoses during that period.
The drastic shift in the American diet has profoundly affected the nation’s health, with diabetes, obesity, and numerous other chronic diseases rising steadily since the 1970s—conditions that fiat scientists and their corporate sponsors conveniently dismiss and pretend are unrelated to diet.

From 2013 to 2021, approximately 11% of U.S. adults were diagnosed with diabetes, reflecting the widespread and growing impact of this chronic metabolic disease.
And the prevalence of cardiometabolic diseases like diabetes and myocardial infarction in the United States underscores the profound health consequences of a food system shaped by fiat currency, centralized banking, and industrialized farming.
As fiat-driven subsidies favor the production of ultra-processed, nutrient-deficient foods such as refined grains, added sugars, and seed oils, these unhealthy products have taken over as common everyday staples in the American diet.

In 2021, it was estimated that a total of 97.6 million adults in the United States had prediabetes, with men accounting for around 53.2 million of these cases. Individuals with prediabetes have blood sugar levels higher than normal, but not high enough to yet be diagnosed with diabetes.
This has fueled a dramatic rise in conditions like diabetes, now affecting 11% of adults, while millions more unknowingly live with prediabetes or insulin resistance—silent conditions that often go undetected for years until they progress into serious health complications.
And as more nations industrialize and adopt fiat currencies and central banking policies, the rise in these chronic diseases in those nations almost becomes inevitable.

The increase in the number of diabetics worldwide between 2021 and 2045, sorted by region. In this period, the number of diabetics in Europe aged between 20 and 79 years is expected to increase ~13 percent. In Africa, by roughly 134%.
Nations transitioning from traditional diets to industrial foods have a high probability of, and should experience rapid increases in obesity, diabetes, and other chronic health issues, mirroring the trajectory of Western countries.
The connection is undeniable: as fiat money expands, so too does the infrastructure that drives the consumption of nutrient-poor, industrially manufactured foods.
And as fiat systems continue to grow, they facilitate the spread of the same subsidies and industrial agricultural practices that have defined the Western diet, accelerating the global proliferation of ultra-processed foods and the rise of chronic disease.

In 2017, around 326.5 million people worldwide aged 20-64 years had diabetes and it is forecasted that this number will increase to 438 million by 2040.
In a recent study, researchers analyzed data spanning from 2002 to 2017.
They examined the number of young people (under 20) with type 1 or type 2 diabetes, and how cases have increased.
Using mathematical models based on these past trends, the researchers were able to predict how many kids and teens will be diagnosed with diabetes by 2060.

Constant incidence: If the rate of new diagnoses stays the same, type 1 diabetes cases would remain about the same. Type 2 diabetes cases would increase about 70%.
Increasing incidence: If the rate of new diagnoses continues to increase, type 1 diabetes cases would increase about 65%. Type 2 diabetes cases would increase about 700%.
The researchers also created a hypothetical model that decreased the annual incidence of type 2 diabetes by 2% through prevention efforts. This model reduced the increase of diabetes in young people to 294,000, compared to 526,000 without prevention efforts.
The Great Faustian Bargain
If you’ve made it this far, you’re likely beginning to see the direct impact of inflation and fiat money on human health.
As paper wealth appears to rise, and technological change continues to accelerate, with hardware becoming faster and cheaper, the nerds have been able to write their code at higher levels of abstraction, allowing for economies of scale.
As we continue to scale, and “food” becomes cheaper and more widely available, nutrient-dense foods have been increasingly replaced with nutrient-poor industrial substitutes, leading to the physical degeneration of man.
If you talk to any American age 70 and up, they will tell you: “back in my day we didn’t have all of these foods.”
But these days, Americans are consuming more highly processed, artificially flavored industrial sludge than ever before.
Today, our fat American bellies no longer serve as symbols of status and wealth, as they did during the European Renaissance and Baroque periods.
In those times, wealthy individuals often commissioned portraits depicting themselves as pleasantly plump to emphasize their ability to afford abundant food, especially while much of the population faced scarcity. Artists like Peter Paul Rubens famously celebrated fuller-figured subjects, giving rise to the term ‘Rubenesque.’
Our modern rise in obesity, however, is not an indicator of abundance but rather a symptom of deprivation.
The level of spending and income in America may be rising according to government stats but working longer hours along with declining basic nutrition suggest deeper issues with the ‘money’ Americans rely on both as a store and measure of value.
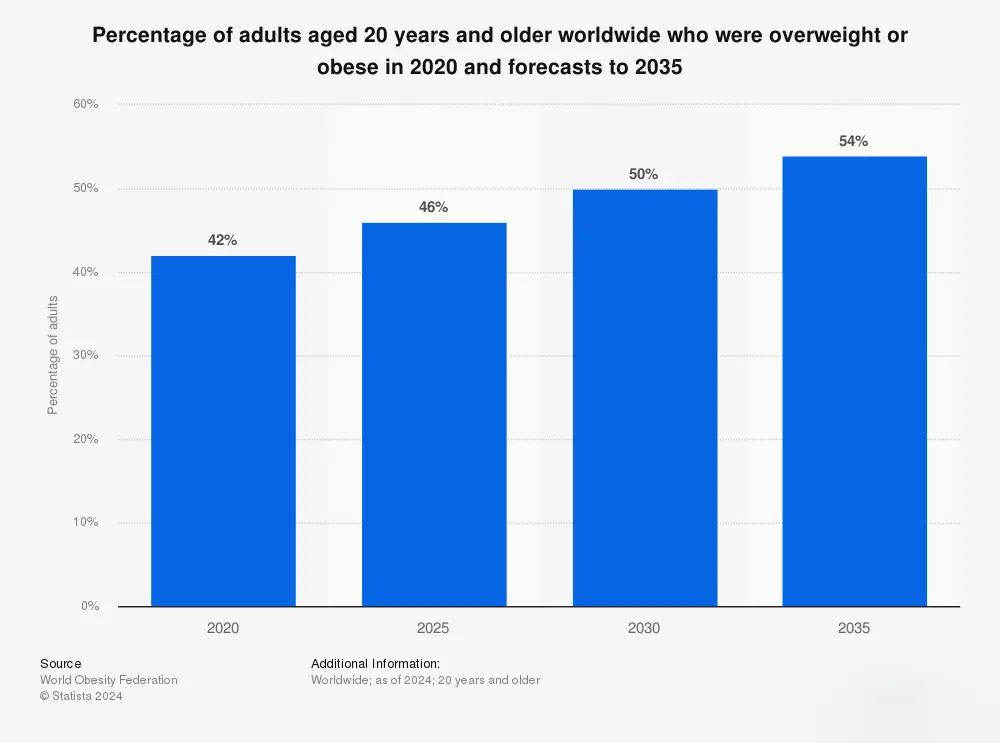
In 2020, around 42 percent of adults aged 20 years and older worldwide were considered overweight or obese. This statistic is projected to rise to 54% by 2035.
The Faustian bargain of fiat currency has not delivered the great and prosperous future its cheerleaders promised, instead it gave the world a dangerous diet full of nutrient-light, high-calorie, industrial concoctions that come at a steep cost to health and well-being.
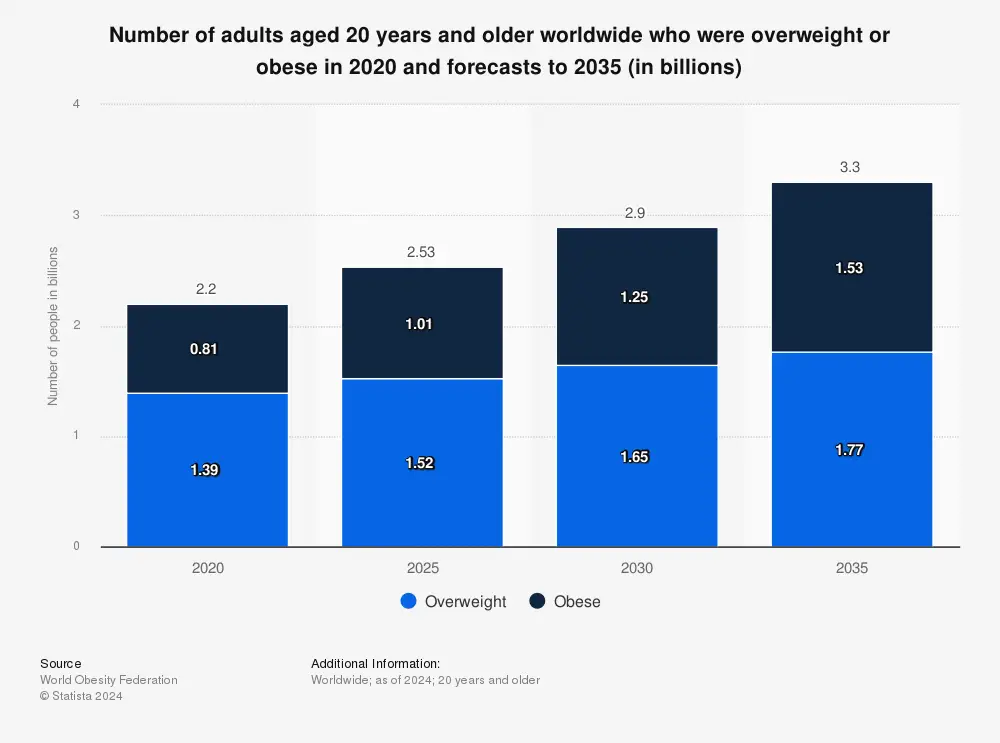
In 2020, around 2.2 billion adults aged 20 years and older worldwide were considered overweight or obese. This number is expected to increase to around 3.3 billion by the year 2035.
The rapidly increasing cost of healthcare and medication cannot be fully understood without careful analysis of the broader degradation of health, diet, and soil, or from the economic system that fuels this crisis.
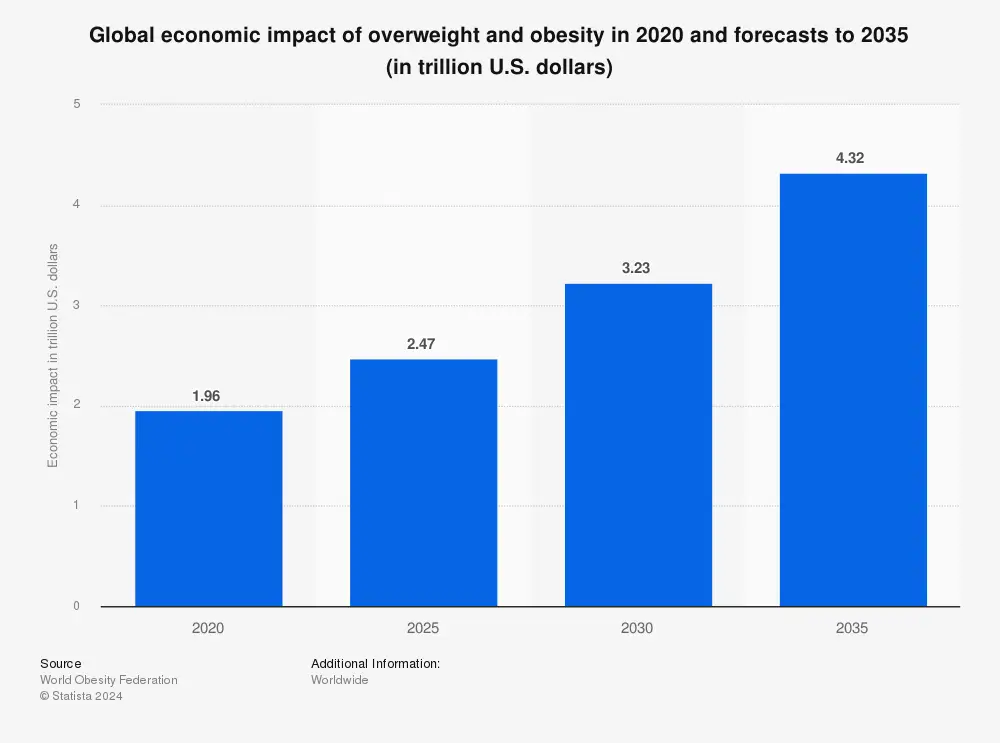
In 2020, the estimated economic impact of overweight and obesity worldwide in 2020 was around $1.96 trillion U.S. dollars. By the year 2035, the economic impact of overweight and obesity is predicted to reach $4.32 trillion U.S. dollars.
The healthcare costs associated with treating these diseases often increase in lockstep with the adoption of fiat policies.
As chronic illnesses become more prevalent, healthcare spending balloons, placing greater financial strain on governments and individuals.
This creates a vicious death-loop cycle: fiat-driven policies subsidize unhealthy food systems, leading to widespread health issues and chronic disease, which in turn demand increased healthcare expenditures—further incentivizing the expansion of fiat currency to fund these costs.
As a result, we are facing an unprecedented obesity crisis in America right now, with more overweight people than ever before.
Fiat funded scientists and state sponsored propagandists have labeled it a crisis of abundance, implying that our affluence has made obesity a greater issue than starvation.
When that doesn’t work, they try to push ‘body positivity’; and while there is nothing wrong with feeling good about yourself, pushing this sort of rhetoric on people, knowing it will likely kill them in the end, should be criminal.
This tragic, self-flattering misrepresentation of the crisis stems from a suboptimal shift in the Overton window and social norms, rooted in a flawed nutritional paradigm—one distorted by intellectual dishonesty and fake science, thoroughly disfigured by government funding and influence.
Within this flawed thesis, calorie quantity is emphasized and eating a “balanced” diet heavy in grains while avoiding “harmful” animal fats in meats is recommended.
In this framework, obesity is simply the result of excess calories, while malnourishment stems from too few—a view as overly simplistic and reductive as the Keynesian textbooks’ assertion that economic health hinges solely on aggregate spending, with inflation caused by excessive spending and unemployment by too little.
After all, it was Keynes’s theories and advocacy for government intervention and deficit spending during economic downturns that laid the intellectual foundation for the modern fiat system.
Today, his ideas continue to shape the world, enabling central banks and governments to ‘print money out of thin air’ to manage economic cycles without being constrained by a gold standard—often at the expense of long-term monetary stability.
This inevitably leads to inflation and currency devaluation.
Author’s note on Keynesian Economics: Keynesian economics (developed by John Maynard Keynes, a power player from the Bretton Woods Conference above) went on to become one of the most influential economic theories of the 20th century, forming the foundation for the current government intervention/central planning model we use in our economy today. Central to Keynesian theory is the idea that, during economic downturns (especially during recessions), governments should use fiscal and monetary tools—like increased spending, tax cuts, or lowered interest rates—to boost aggregate demand, reduce unemployment, and prevent economic stagnation. This theory underpinned much of the economic policy in Western countries post-World War II, but especially in the U.S., where it most significantly influenced fiscal policy, social spending, and employment programs. Over time, Keynesian ideas evolved into Neo-Keynesian and New Keynesian frameworks, which played a huge role in central banks’ use of interest rates and policies like quantitative easing. Keynesian principles also shaped global institutions like the IMF and World Bank (as discussed above), promoting counter-cyclical policies that adjust government spending based on the economic cycle, especially during crises, to maintain stability and growth.
In macroeconomics and political theory, there are two prominent and conflicting schools of thought: the Austrian School of Economics and Keynesian School of Economics, especially when it comes to the role of government in the economy.
The Austrian school argues against government intervention, advocating that economic cycles are natural consequences of individual preferences and time-value considerations. Austrian economists attribute recessions to credit expansions from central banks, leading to “malinvestment” (misallocation of capital), which must eventually correct itself through market-driven recessions. In terms of political theory, the Austrian school leans toward classical liberal or libertarian ideas, prioritizing individual liberty, property rights, and minimal state interference. They believe that government interference, even for stabilization purposes, tends to distort markets and lead to inefficiencies or even crises.
On the other hand, the Keynesian school is more statist-leaning, and supports a more active role for government, especially during economic downturns. Keynesians argue that government spending can stimulate aggregate demand and pull an economy out of a recession. They view fiscal and monetary policy as tools for achieving full employment and economic stability, advocating that without intervention, economies can remain under capacity for long periods. As such, Keynesianism political theory generally supports a more centralized, interventionist state, with a social contract focused on managing demand to ensure economic stability and job security. This aligns more with social-democratic or interventionist political ideals that advocate a significant role for government in economic and social welfare.
We see these two schools clash not only in American politics, but in politics across the world. Of course there is some crossover, but the Austrian school leans toward minimal government, individual autonomy, and a free-market system with voluntary exchanges as the foundation of both economics and civil society. The Keynesians see the government as a necessary stabilizer, using policy to address issues that pure markets can’t solve, such as unemployment and poverty, while aiming for equitable economic outcomes.
There is a fundamental ideological split between the free-market individualism of the Austrians and the state-managed economy of the Keynesians. Many modern economic theories borrow from both, as the challenges of today can be more nuanced, but the little talked about Austrian-Keynesian divide remains a central debate on economic philosophy and governance.
So, the next time you’re watching the news or see a news report quoting an ‘expert economist,’ take a moment to consider which school of thought this so-called expert was trained in—and how zealously they cling to its dogma—it will likely explain exactly why they said what they did.
Nutritional Poverty Starts with Deficiency
If you’ve followed this blog over the years, you’ll know that nutrition involves a lot more than basic caloric intake; it’s about securing adequate amounts of essential nutrients across four primary categories:
- Proteins
- Fats
- Vitamins
- Minerals
Protein builds and repairs tissue and supports various enzymatic and hormonal functions.
Fats supply energy and are important for cell structure, hormone production, and nutrient absorption.
Vitamins and minerals support biochemical processes necessary for overall health.
While carbohydrates can also provide energy, they are much less essential for human survival, as the body can produce glucose through gluconeogenesis from proteins and fats.
However, prolonged deprivation of essential nutrients—such as amino acids, fatty acids, vitamins, and minerals—the body suffers and deteriorates, resulting in disease and dysfunction.
Notably, without animal proteins and fatty acids, the body is forced to enter a starvation state, reducing energy expenditure, which often manifests as physical and mental lethargy and inactivity.
In this state, the body converts ingested carbohydrates into fatty acids for future use—and if you eat too many carbs, it can result in obesity.
Contrary to popular belief, obesity is not a sign of affluence but rather a symptom of malnutrition.
The ability to store fat by converting plant-based carbohydrates into stores of fatty acids is a very useful evolutionary advantage during short-term food scarcity, but chronic deprivation of essential nutrients can transform that fat storage into the illness of obesity.
So, rather than being a sign of wealth and overconsumption, obesity reveals an unmistakable sign of nutritional poverty and malnourishment.
How do you reverse the cycle?
Millions of people across the world (including myself) have improved their health immensely simply by avoiding all processed fiat foods.
While the specific diet plans may vary, the common theme of any successful diet is the reduction, and, eventually, the total elimination of these heavily processed foods.
Thanks to the internet and social platforms like Twitter/X, many people are able to share their experiences outside the watchful eye and constraints of the fiat scientific establishment, leading to a new, experience-based consensus—one that is much different than what’s endorsed by the fiat authorities.
While medical schools, nutrition experts, and government propagandists continue to rationalize and promote the consumption of industrially processed “sludge” under the guise of “balance”, online communities have helped millions all over the world reclaim their health by getting back to the basics and avoiding the fiat recommendations.
If you forget everything else you read here today, remember this one critical point: Decepticon intellectuals come in many forms.
But one of their most common tricks is to play the role of the expert.
Bold predictions.
Fancy charts.
Long exposition.
Pseudo quant.
Devoid of logic.
Immovably committed to bold positions because it makes you sound smarter than being humbly realistic.
A clever trick to gain erroneous credibility and praise.
But most of them do not have a clue.
Because they are simply actors.
Actors who play experts on TV.
Their job is to scam you into buying into the local kleptocracy’s fiat Ponzi scheme.
That said, the state of nutrition is analogous to the state of economic research: a fiat-funded mainstream heavily focused on arriving at the conclusions that support its fiat financing.
Just like economics has had honorable theorists like Mises, nutrition also has deep thinking, independent voices. While the field of nutrition has devolved into a junk food marketing machine, renegades are beginning to challenge the dominant narrative.
John Yudkin’s valiant but ultimately unsuccessful fight against sugar is a classic case, yet the most comprehensive approach to studying nutrition may come from the work of Canadian dentist Weston Price, who, nearly 100 years ago, theorized a framework for understanding health based on whole, unprocessed foods.
Price is mostly known today for his work in early vitamin research, as well as his groundbreaking work about the link between diet and health in his book Nutrition and Physical Degeneration.
His meticulous, worldwide study of isolated, traditional societies—conducted just as air travel was emerging—allowed him to document diets and health outcomes largely untouched by industrial foods.
Unlike today’s mainstream nutritional science—which is heavily influenced by government fiat and special interest groups—Price’s work challenged conventional wisdom: he found no society thriving on plant-based diets alone, observing that the healthiest populations heavily and universally relied on animal fats and proteins.
His findings suggest that malnutrition, obesity, and modern diseases are tied to industrial foods, especially processed grains and sugars, which were virtually absent in traditional diets.
Price noted that traditional food preparation techniques, such as soaking and fermenting, made plant foods safe and nutritious—a labor-intensive approach largely abandoned in the era of high time preference, and quick, industrial processing.
As modern nutrition science increasingly promotes cheap, industrial foods and shuns animal products, Price’s work stands as a counterpoint, illustrating how diets rich in animal foods provide essential nutrients absent in processed alternatives.
Price’s work offers a rigorous and technically sound scientific exploration of the damage caused by modern industrial foods, whose producers are primary benefactors of nutrition schools all over the world.
In addition to being well-documented and methodically thorough, Price’s research is unique and will be difficult to replicate.
He made a massive contribution to our understanding of health and nutrition, but similar to Mises and Menger in Economics, his teachings are largely ignored by the government-employed bureaucrats pretending to be modern scientists.
To no one’s surprise, the book is largely ignored by mainstream academia and nutrition science because his conclusions directly contradict with the politically correct dogma taught in universities today.
How To Rebalance & Restore
In the previous sections, we discussed some of the broader forces and econopathogenic phenomena that have shaped our current health landscape, contributing to the suboptimal health outcomes we see in America today.
Most notably, how central banking practices (e.g., fiat money, fiat science, and fiat foods), corporate incentives, and government propaganda have converged to create suboptimalities in physical and mental well-being and accelerated the rates of chronic illness.
Now, let’s into the next logical step: how we can actively work to reclaim our health.
While the degeneration of our physical well-being is a huge buzz kill, it’s still well within our power to reverse these trends.
The journey to healing begins with informed, “rebellious” lifestyle, diet, and mindset choices that may defy mainstream conventional “wisdom”.
The following section will outline actionable steps to optimize your health and prevent future disease, focusing on ancient, natural methods that align with human biology.
Let’s dive in.
The first step is understanding bio-individuality.
What is bio-individuality?
Bio-individuality is the concept that every person has a unique biological and genetic makeup, leading to individual differences in nutritional and lifestyle needs.
This means that what works well for one person in terms of diet, exercise, or health practices might not be effective—or could even be harmful—for another person, emphasizing the notion that health and wellness are not one-size-fits-all.
Factors influencing bio-individuality include genetics, microbiome diversity, metabolic rate, blood type, age, gender, personal health history, and a few other less critical variables.
That said, we are all human, so we are all remarkably similar at the genetic level, sharing about 99.9% of our DNA with each other.
The remaining 0.1% accounts for all of our individual differences, influencing everything from physical appearance to susceptibility to certain diseases, but more specific to this analysis, the way we respond to our energy sources: carbohydrates and fats.
So, in terms of bio-individuality, our variations in genes will influence our individual metabolic responses to food. Your genetic makeup influences nutrient metabolism, meaning some individuals may require higher (or lower) intakes of certain nutrients to meet their unique physiological needs.
Japanese individuals, for example, often have a variation in the AMY1 gene, which enhances starch digestion efficiency, and may help explain their success with a high-carbohydrate diet.
Studies have also shown that European agriculturalists, Central American, and Middle Eastern groups, populations with traditionally starch-rich diets, have a higher number of AMY1 copies compared to populations with lower-starch diets.
Now, let’s move on to protein, carbs, and fats.
Each of these macronutrients has a different thermic effect of food (TEF), which is the energy expended to digest, absorb, and process each macronutrient:
- Protein has the highest TEF, with roughly 20–30% of its calories used in digestion and processing.
- Carbohydrates have a TEF of about 5–10%.
- Fats have the lowest TEF, at around 0–3%.
Unless you’ve been living under a rock, chances are you’ve come across a fitness account on Instagram at some point. So, you’ve probably heard people say stuff like, ‘You’ve got to eat more protein’ or ‘Eat 1 gram of protein for every pound of body weight.’
But here’s the catch:
For every 100 calories of protein, only about 70 are usable—the rest are burned off and don’t count.
So, ‘eat more protein’ isn’t always good advice.
In fact, it can be dangerous advice depending on the person.
I see people over-consume protein all the time because they’re either following an extreme bodybuilding diet or a distorted oversimplification of a ‘Primal Diet/Primal Lifestyle’ approach, like the one used in the carnivore diet.
Sure, I know many readers might be eager to bulk up, but even an underweight person can over-consume protein.
This excessive intake can lead to elevated ferritin (iron) levels and low uric acid, which are potential indicators of kidney stress resulting from the increased protein load.
So, eating 300 grams of protein a day when you only weigh around 80 kilograms, for example, may be a recipe for disaster.
Let’s pivot back to the thermic effect of food (TEF) for a moment.
Using TEF, we see that 20-30% of the calories in protein are burned during digestion, making protein a more metabolically ‘expensive’ food compared to fats or carbs.
For energy efficiency, however, carbs and fats may be more effective sources, as they require less energy to digest and absorb.
Depending on your genetics and activity level (e.g., high-performance athlete, or casual office Joe), the amount of carbs you’ll need each day will vary.
They are ‘essential’, but you probably don’t need as many carbs as you think, especially if you’re trying to (1) lose weight; and (2) prevent or reverse chronic disease. I will discuss this in more detail shortly.
That said, if you avoid or limit carb intake, your body will derive them from the breakdown of other sources through a process called gluconeogenesis.
Gluconeogenesis is a metabolic process where the body creates glucose from non-carbohydrate sources, such as amino acids (from protein), lactate, and glycerol (from fats). This process primarily takes place in the liver (and to a smaller extent, the kidneys) and is essential for maintaining blood glucose levels, especially during periods of fasting, intense exercise, or low-carbohydrate intake.
This is how Angus Barbieri, who completed the longest recorded fast (382 days), maintained stable blood glucose levels throughout—without eating carbs.
His body sustained necessary glucose through gluconeogenesis, generating it from amino acids and glycerol, which allowed him to function normally during his fast of over a year.
Now, let’s refer back to the food pyramid we discussed earlier.
You’ll recall that fiat scientists and government propagandists have notoriously emphasized ‘calories’ and ‘balance’ and ‘avoiding fat’ in their dietary recommendations—a simplistic approach that promotes calorie counting and assigning specific percentages of calories to each macronutrient.
The government’s macronutrient distribution generally followed these guidelines:
- Carbohydrates: 50-60% of daily calories (primarily from grains, fruits, and vegetables)
- Fats: 20-35% of daily calories (mainly from plant-based oils, nuts, and seeds, with limited saturated fat)
- Protein: 10-20% of daily calories (from meat, fish, poultry, eggs, beans, and nuts)
And they revised it in 2011 with MyPlate.
The MyPlate approach, which the government introduced by the USDA in 2011, eliminated the macronutrient approach and replaced it with a visual guide that looks like a plate.
Here’s the basic breakdown:
- Vegetables: About 30% of the plate
- Grains: About 30% of the plate
- Protein: About 20% of the plate
- Fruits: About 20% of the plate
- Dairy: A small side portion (such as a cup of milk or yogurt)
Contrary to the gross oversimplification that is the MyPlate approach, I generally recommend significantly lowering carb intake, increasing fat intake, and eating moderate amounts of protein.
And the specific amounts of each macronutrient should be aligned with individual health and metabolic needs
Why do I recommend eating more fat?
Because fats (the healthy fats) help with:
- Energy storage and production
- Brain health
- Gene expression
- Blood clotting
- Cholesterol balance
- Mood and mental health
- Hormone synthesis
- Vitamin absorption
- Satiety and taste
Now, before we get to the good stuff, it’s important that you first understand the concept of ‘metabolic flexibility’, which refers to the body’s ability to efficiently switch between using carbohydrates and fats for energy based on availability and demand.
When the body is metabolically flexible, the body can adapt to different fuel sources depending on factors like activity level, fasting, and diet composition, optimizing energy production without fatigue or energy crashes. This flexibility is associated with improved insulin sensitivity, stable blood sugar levels, and overall metabolic health.
The human body is an intelligent machine and metabolic flexibility allows the body to seamlessly switch between using carbohydrates and fats for energy based on our daily rhythms and energy demands.
During the day, when we’re more active, the body often prefers carbohydrates as its primary fuel source, tapping into stored glycogen for quick, accessible energy to support movement and focus.
At night, however, when our activity levels drop and we enter a fasting state, the body naturally shifts to burning fat for energy.
This day-to-night energy shift supports stable blood sugar, balanced energy, and optimal metabolic health.
I’ll explain how to achieve this in a bit, but for now, let’s talk about what to eat.
Here are my general recommendations:
- A diverse animal-based intake
- Healthy fats
- Natural, whole foods
- Seasonal, local foods
- Hydrating foods
- Diverse fiber sources
- Fermented foods
- Minimal ingredients
Veganism or avoiding vegetables altogether is a big no-no.
People who only eat vegetables or never eat vegetables often have nutritional deficiencies and sustained illness, but this is a topic for another day.
Here is your new grocery list:
Recommended Protein (farmers market or butcher)
- Grass-fed beef (variety of cuts, biltong, mince)
- Salmon, white fish, tuna
- Pasture-raised eggs
- Oysters
- Raw milk
- Whole yogurt
- Collagen
I used to eat chicken but no longer recommend it as part of a healthy diet. Chicken, particularly when grain-fed, is high in inflammatory omega-6 polyunsaturated fatty acids (PUFAs). Excessive omega-6 intake has been linked to inflammation and diabetes.
As I mentioned earlier, one of the simplest and most effective ways to improve your health right away is to avoid all processed fiat foods, particularly PUFAs (polyunsaturated fatty acids). One of the worst offenders here is linoleic acid, an Omega-6 PUFA found in high amounts in vegetable and seed oils.
If you’re looking for a starting point to improve your health, my top recommendation is to eliminate PUFAs from your diet—especially linoleic acid, which is heavily present in seed oil.
Well guess what, the biggest source of Omega-6 in the American diet is chicken.
That’s right, chickens are vehicles for PUFAs, meaning, when they eat PUFAs in their feed, their fat will have more PUFAs.
I’m not sure how many folks out there have ever farmed chickens, but you could make the case that 99% of chicken feed in America is PUFA rich (including most of the ‘corn & soy free’ brands out there).
Also taking into account the vaccines (both standard and mRNA), the chlorine baths, and the dirty close quarters, chicken makes it to the top of my ‘foods to avoid’ list.
Recommended Healthy Fats:
- Extra virgin olive oil
- Coconut oil
- Butter
- Tallow
- Ghee
- Cheese
- Avocado
- Flaxseed/chia
- Nuts/Nut butters
Avoid these oils: Canola, Corn, Cottonseed, Grapeseed, Rice bran, Safflower, Soy, Soybean, and Sunflower. Get them out of your kitchen.
Recommended Carbohydrates:
- Steel cut oats
- White jasmine rice
- Sweet potatoes/potatoes
- Squash/pumpkin
- Cauliflower
- Leafy greens
- Organic fruit
- Raw honey
- Various veggies
Recommended Miscellaneous:
- Sea salt
- Bone broth
- Kimchi/sauerkraut
- Kefir
- Apple cider vinegar
- Cacao
- Ginger/Garlic
- Lemon
- Stevia (liquid is optimal)
Author’s note: If you have insulin resistance, which I will discuss in detail later in this text, you should restrict or avoid carbohydrate/sugar intake until the problem is resolved. This process can take anywhere from 6 to 60 months depending on the severity.
Author’s note: I recommend avoiding gluten whenever possible, especially processed gluten (e.g., white bread, dry pasta, pastries, etc.). It triggers the protein zonulin, which increases intestinal permeability (leaky gut). I have written extensively about zonulin and leaky gut here.
Author’s note: Sodium is commonly demonized, but it is essential for hydration and cellular function/optimization. Sodium and glucose in a ratio of at least 2:1 activate sodium-glucose transporter proteins (SGLTs), which facilitate the movement of water across cell membranes. You need both sodium and glucose to efficiently transport water into cells and maintain electrolyte balance. There are some healthy sodium sources in our grocery list above but some other sources include: celery, beets, swiss chard, seaweed, and olives.
Now to answer your next question: how to eat for optimal health and human performance?
There are no absolutes when it comes to your health, but here is a strategy that works very well:
- Fast until 12-2pm
- Stay low carb until 3 or 4pm (a piece of fruit is OK)
- Have your highest carb meal 2-3 hours before bed
- Optimize for protein in every meal
- Make sure you get enough healthy fats in every meal to prevent snacking on junk food between meals
- Walk after each meal
- Consistent medium-intensity fasted training
If you are insulin resistant or have poor insulin sensitivity—which many Americans do—it’s critical to work on making your cells more receptive to insulin.
The most effective ways to do this are through fasting and carbohydrate restriction, as both can reduce insulin levels and help the body better manage blood glucose.
Then, once your system is functioning better, gradually increase your carb intake over time.
Here are a few more simple steps to take:
Time Restricted Eating (TRE)
TRE is arguably the biggest factor to improving insulin sensitivity.
- Start with a 12-hour fasting window
- Gradually increase to 14-16 hours
- Eventually build up to a full 72 hour fast
This will train your body to use fat as a fuel source again.
I will discuss fasting in more detail below but here are some general guidelines:
1) Manage Carb Intake
Eating fewer carbs = less blood sugar.
Less blood sugar = lower insulin.
Low-carb interventions alone have been shown in studies to take people off hundreds of units of insulin in just weeks (not good for fiat pharma).
I recommend limiting carbs to 50-100g per day.
Also, if you’re an analytical person, you may want to invest in a glucose meter and start checking your blood sugar before and after meals. The goal should be to maintain a healthy baseline and never try to exceed a 30-point blood sugar spike after meals.
2) Eat More Red Meat
- Steak is an absolute must for peak health and performance.
- It’s a superfood that’s packed with nutrients.
- The fatty acids in steak can reduce cravings by promoting satiety, stabilizing blood sugar.
- More steak = more muscle, and muscle is a sponge for blood sugar.
3) Walk After Meals
This will lower post-meal blood sugar spikes.
I recommend walking for at least 5 minutes after every meal, but especially after meals including carbs.
Start slow (5 minutes is better than nothing) and work your way up to a 1 hour walk each day.
4) Eat More Fiber
Try to get 30-40 grams per day.
What should you eat?
Whole foods and nutrient-dense plants like:
- Almonds
- Apples
- Artichoke Hearts
- Avocado
- Broccoli
- Carrots
- Cauliflower
- Chia Seeds
- Coconut Meat
- Dragon Fruit
- Flaxseeds
- Pears
- Pecans
- Raspberries
- Spinach
- Strawberries
- All Vegetables
5) Lift Weights
You don’t need to dedicate your life to the gym to reverse insulin resistance, get lean, or improve your health.
You just need to do enough to trigger muscle building and fat burning.
2 to 3 times a week will be enough if you: use a full-body split, pick the proper exercises, and train to failure.
If you need a new workout plan, there are a bunch of free workouts on The Unconquered Mind that you can try.
6) Get Sunlight & Sleep
Sunlight provides vitamin D and enhances insulin sensitivity.
Sleep lowers cortisol and helps sugar metabolism.
This combo packs a powerful punch in the fight against insulin resistance.
Make sure to get:
- 10-15 minutes of morning sun
- 30 minutes of total sun time daily
- 7+ hours of sleep a night
Here are 7 tips for better sleep:
- Move every day (walk, run, lift)
- No caffeine after 12pm
- Avoid naps after 2pm
- Block blue light before bed
- Wake and sleep at the same time each day
- Create a sleep cave: quiet, dark, cold
- Invest in a good mattress
- Wakeup:
- Methi Dana (soaked overnight in water). Before you go to bed put 2 tsp of Fenugreek powder or seeds in 4-6 ounces of water. Drink the water and the seed mixture in the morning. After you finish it, drink one bottle of purified water.
- Morning tea: Ayurvedic Detox (1tsp Alma powder + 1/4 tsp Turmeric powder + 1/4 tsp Jamun powder). Mix in hot water and drink on an empty stomach.
- Morning supplement: D3/K2 on an empty stomach.
- Morning walk: 5 minutes and work your way up to 1 hour.
- Taken with first meal (eaten between 12-2pm):
- Berberine (helps control appetite and regulate blood sugar)
- Milk Thistle (cleanses liver so it stops releasing too much glucose)
- PQQ (improves brain function and works in tandem with berberine)
- Blackseed Oil (anti-inflammatory to heal the insides from the glucose and fatty tissue damage)
- Meal 1 (2pm):
- 10-12oz ribeye steak. large salad, avocado, sea salt.
- Homemade salad dressing: 2 tbsp extra virgin olive oil + 2 tbsp bragg apple cider vinegar + 1 tsp whole grain mustard + dash of garlic powder
- Meal 2 (6pm):
- Norwegian salmon, salad or green veggies, avocado, raw cashews.
- Monitor Your Blood Sugar: Test your blood sugar before each meal, 30 minutes after eating, and 2 hours after to see how different foods affect you. This is a must even if you don’t have diabetes, since blood sugar is a leading indicator for every major disease. You can find an affordable glucose monitor at your local drugstore or talk to your doctor about a continuous glucose monitor (CGM).
- Control Blood Sugar Spikes: Aim to keep post-meal blood sugar spikes under 30 points. If it exceeds this, adjust your food choices. If you have insulin resistance, cutting carbs and sugar to near-zero may be necessary. Replace those calories with healthy fats and proteins like ribeyes, avocados, olive oil, nuts, and seeds.
- Minimize Carbs: Reduce carbs as much as possible and be cautious of hidden carbs in packaged snacks. Read all labels. Only eat foods tested with your glucose monitor.
- Cut Liquid Sugar: Skip sugary drinks and make stevia lemonade at home by mixing unsweetened lemon juice, cold water, and a few drops of stevia.
- Prioritize Daily Walking: Walk 2-3 miles daily, or at least take a 5-minute walk after every meal to support blood sugar regulation. This is essential—don’t skip it.
- Avoid Self Inflicted Injury: Eliminate drugs, alcohol, smoking, and vaping entirely.
- Try Ancient Healing Elixirs: Before carb heavy meals, mix 1/2 tsp of Jamun seed powder in 4-6 oz of hot water and drink it like tea.
- Get Off Your Ass: Movement is critical. Aim to lift weights and do cardio at least 2-3 times a week for overall health and fitness.
- Everything Starts Here: Take a digestive enzyme supplement with every meal, especially those containing carbs, to aid digestion.
- Don’t Forget About Gut Health: Invest in a high-quality probiotic and take it at night before bed.
- Boost Immunity: Take zinc, quercetin, and magnesium before bed to support immunity, relaxation, and overall health.
- Focus on Blood Pressure: Consider experimenting with L-Arginine, which may help manage blood pressure.
Insulin Resistance Explained
If there’s one critical factor that’s consistently overlooked yet arguably the most important in determining human health and risk of death, it’s insulin resistance.
Insulin resistance is a silent, asymptomatic ‘killer’ that gradually weakens vital systems in the body over time, ultimately contributing to many of the leading diseases in America today, including metabolic syndrome, obesity, type 2 diabetes, cardiovascular disease, non-alcoholic fatty liver disease, and many other chronic maladies.
Millions of people in America are currently walking around feeling fine, completely unaware that they are either pre-diabetic or already living with insulin resistance.
I highly recommend getting bloodwork done at least once a year to monitor your fasting glucose and A1C levels to see where you’re at. This will give you a baseline for your metabolic health so you’ll know what to work towards.
If seeing a doctor isn’t an option, there are alternative methods to assess whether you might be insulin resistant or borderline:
- Do you ever get hunger pangs even after you just ate?
- Does your gut somehow always seem to grow no matter what you try?
- Do you experience brain fog?
- Does the brain fog ever get so bad it feels like you can’t even think?
- Do you experience mood swings at the tiniest things for no apparent reason?
- Are you fighting constant fatigue every day, even if you slept a good 7 or 8 hours the night before?
If so, it’s because modern life is a breeding ground for insulin resistance.
Desk jobs, high-stress work, sedentary lifestyle, lack of sunshine, and sleep deprivation team up with diets heavy in seed oils, processed foods, refined grains, and sugars to create the ultimate recipe for insulin resistance and chronic disease.
But first, what is insulin resistance?
Insulin resistance is a condition where the body’s cells become less responsive to insulin, resulting in higher blood glucose levels and requiring more insulin to achieve the same effect.
When the body is insulin resistant, the cells lose their ability to absorb glucose from the bloodstream effectively, leading to elevated blood sugar and higher insulin levels as the body tries to compensate.
Think of insulin as a hormone that works like a key, putting sugar into your cells. When there’s insulin resistance, the key doesn’t fit right.
The sugar can’t get into your cells, so it builds up in the blood.
It’s like a door that’s jammed.
This leads to chronic inflammation, which causes: fatigue, brain fog, joint pain, and fat gain.
Then eventually, the 4 Horsemen of Chronic Disease:
- Heart Disease
- Cancer
- Diabetes
- Alzheimer’s
Heart disease is the #1 killer.
But it’s insulin resistance that causes it, along with cancer, diabetes, and Alzheimer’s.
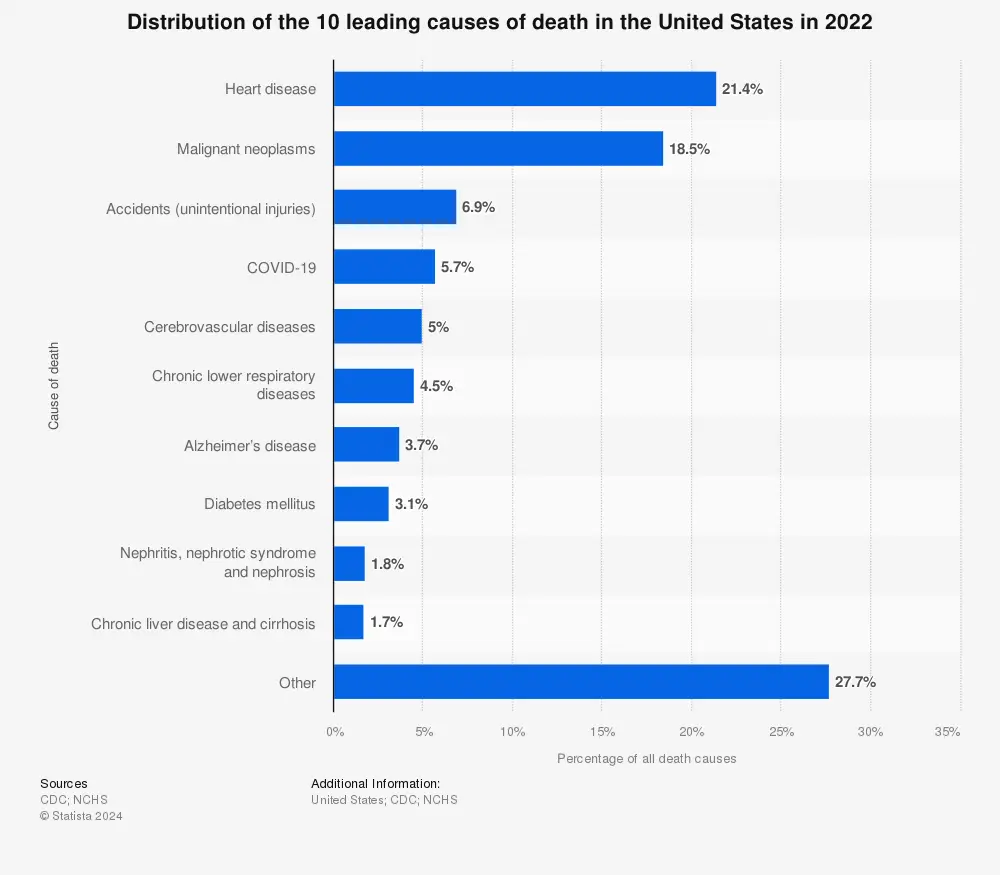
Heart disease is the leading cause of death in the United States. In 2022, COVID-19 was the fourth leading cause of death in the United States, accounting for almost six percent of all deaths that year.
Author’s Note: Recent research has explored the concept that cognitive disorders like Alzheimer’s disease may be linked to insulin resistance in the brain, leading some to refer to Alzheimer’s as “type 3 diabetes.
But don’t stress…
Despite what “experts” say, insulin resistance is completely reversible.
But your doctor isn’t going to help you reverse it, you’ve got to take matters into your own hands.
In the following section, I’m going to outline some simple steps that can help you turn things around. But first, here are some general observations:
1) Insulin resistance stems from poor metabolic health.
2) Insulin resistance can develop without being overweight.
3) Type II diabetes is essentially an advanced form of insulin resistance.
4) Inactivity and obesity are the leading contributors to insulin resistance.
5) Children of insulin-resistant parents are more likely to develop insulin resistance due to shared lifestyle habits.
6) Insulin resistance increases risk for hypertension, type II diabetes, mortality, various cancers, and Alzheimer’s.
7) Heart disease is an inflammatory process kicked off by insulin resistance, not meat or cholesterol.
8) Cardiologists were once rare, as heart disease is largely a modern issue linked to fiat foods and being lazy.
9) You can be insulin resistant without any symptoms, since it’s a leading indicator and blood sugar is a lagging indicator.
10) When you eat, your pancreas releases insulin to move glucose from your bloodstream into muscle, fat, and liver cells.
11) If blood sugar remains elevated (often due to a diet high in refined carbs and sugars), the pancreas must produce more insulin consistently to keep up with demand.
12) As the pancreas produces more insulin to compensate, inflammation in the body increases.
13) Over time, cells (especially in muscle, liver, and fat tissue) become less responsive to insulin due to the constant exposure to high insulin levels. This desensitization reduces glucose uptake by cells.
14) As cells resist insulin, the pancreas compensates by producing even more insulin to try to lower blood glucose, resulting in hyperinsulinemia.
15) The liver and fat cells may convert excess glucose into fat, leading to weight gain and inflammation, which further impairs insulin sensitivity.
16) This cycle continues as the cells grow increasingly resistant, requiring even more insulin to lower blood glucose.
17) With chronically high blood sugar, your body requires more insulin to achieve the same effect, similar to tolerance in drug use.
18) Consistently elevated blood sugar eventually leads to prediabetes or type II diabetes if left unchecked.
19) Type II diabetes results from the pancreas being unable to produce sufficient insulin, though damage begins well before.
20) Consistently high blood sugar damages blood vessels and leads to energy crashes when insulin spikes to clear excess sugar.
21) Insulin is primarily triggered by carb intake, as carbs are quickly broken down into glucose, signaling the pancreas to release insulin, raising blood sugar levels.
22) Refined grains/carbs, such as bread and pasta, break down rapidly into sugar in the bloodstream.
23) While carbs aren’t problematic for everyone, those with insulin resistance or type II diabetes should focus on reducing carb intake until levels stabilize.
24) Over 88% of Americans are metabolically unhealthy based on blood pressure, blood sugar, triglycerides, or waist size.
25) A waist measurement over 40 inches for men is linked to insulin resistance, and 40 inches happens to be the average waist size for men over 25.
26) A high omega-6 to omega-3 fatty acid ratio is associated with increased inflammation and disease risk.
27) Seed oils, such as canola and soybean, are high in omega-6s and widely used in processed foods due to cost and long shelf life.
28) People with heart disease have higher linoleic acid in their fat tissues; linoleic acid makes up 20-70% of seed oils like canola/sunflower/soybean/corn.
29) Inflammation in blood vessel walls can lead to blockages, increasing the risk of heart attacks and strokes.
30) Abdominal fat and insulin resistance cause organ inflammation, which can increase cancer risk.
31) Insulin resistance can be prevented or reversed with fasting, weight lifting, weight loss, regular activity, and avoiding processed foods.
32) Reversing insulin resistance boosts energy, reduces junk food cravings, improves mental health, and extends lifespan.
33) Eating more eggs and fewer refined carbs at breakfast can improve HDL (good cholesterol) and lower triglycerides.
34) Sun exposure has been shown to reduce insulin resistance, insulin levels, and triglycerides in diabetic patients.
35) High-protein diets are inversely associated with insulin resistance.
36) Fasting has been shown to improve glucose control, gut health, and insulin sensitivity.
37) A high triglyceride-to-HDL ratio is one of the strongest indicators of mortality risk.
38) A low triglyceride-to-HDL ratio greatly reduces mortality risk, with both markers improving alongside metabolic health.
39) Resistance training increases HDL and reduces triglycerides and blood sugar levels.
40) Strength-trained seniors can have greater muscle strength than inactive young adults; resistance training promotes healthy aging.
41) Muscle mass lost due to aging negatively impacts insulin sensitivity, but resistance training can counteract it.
42) Exercise helps muscles absorb blood glucose and use it for energy.
43) Walking for just 5 minutes before or after meals helps stabilize blood sugar.
44) Muscle tissue is highly metabolically active; building muscle enhances insulin sensitivity.
45) Added sugars and refined grains are strongly linked to insulin resistance.
46) Consuming liquid calories can lead to poor metabolic health.
47) Choose whole foods: meat, eggs, dairy, and vegetables.
48) When in doubt, eat farm foods. Meat, eggs, dairy and whole vegetables.
49) Resistance training builds and preserves muscle, especially important in older adults.
50) While exercise is crucial, an active lifestyle is just as important. Walk, bike, play with your kids, take the stairs, and set goals like a 5K to stay motivated.
51) Advanced insulin resistance can be reversed with the right mindset, plan, and lifestyle changes, though it becomes harder the longer it’s left untreated.
The Miracle of Fasting
Fasting has been practiced by humans for thousands of years, with its roots tracing back to early hunter-gatherer societies who naturally fasted due to limited food availability and scarcity.
As civilization progressed, fasting became an intentional practice for physical and spiritual health, with recorded instances in ancient Egypt, Greece, and India.
The legendary Greek physician Hippocrates, often called the “Father of Medicine,” advocated fasting as a way to heal the body, while many religious traditions (e.g., Hinduism, Buddhism, Christianity, Islam) incorporated fasting as a discipline for spiritual growth and physical purification.
Fast forward to today and science has validated the benefits of fasting for metabolic health, particularly in addressing conditions like insulin resistance.
By giving the digestive system a rest, fasting allows the body to shift from glucose dependency to fat burning, improving blood sugar regulation and supporting weight loss and cellular repair.
Additionally, fasting triggers autophagy, a cellular repair process that removes damaged components, while increasing the production of human growth hormone (HGH), which preserves lean muscle mass and aids metabolic health.
Based on the latest research, you must fast at least 48 hours to achieve meaningful effects and 72 hours to achieve better outcomes (e.g., resetting your immune system, eliminating cancer cells, protecting your cells from chemo induced DNA damage).
Fasting not only offers profound metabolic benefits but also plays a significant role in resetting the immune system and enhancing its ability to fight diseases, including cancer.
Unlike short-term ketogenic diets or calorie restriction, fasting is more potent in triggering protective cellular mechanisms.
One of its key effects is the dramatic reduction in IGF-1 (insulin-like growth factor), a hormone that regulates cell growth and metabolism.
By lowering IGF-1 levels, fasting protects normal cells from stress and damage while simultaneously sensitizing cancer cells to chemotherapy, making treatments more effective.
Fasting is much more powerful against cancer than short-term ketogenic or calorie-restricted diets because it lowers IGF-1 (insulin-like growth factor) and produces ketones, which starve cancer cells while protecting healthy ones.
Studies have shown that this process is key to protecting normal cells and simultaneously sensitizing cancer cells to chemo.
Furthermore, prolonged fasting (48-72 hours or more) has been shown to promote the regeneration of immune cells by stimulating stem cell activity, helping the body to rebuild a stronger and healthier immune system.
This dual ability to shield healthy cells while targeting abnormal or diseased cells underscores fasting’s powerful role in both immune system resetting and cancer therapy.
The timeline below illustrates the progressive physiological changes that occur during fasting, highlighting the body’s remarkable ability to heal and adapt over time.

A general breakdown of common physiological changes associated with fasting. The specific timeline of events and percent change will vary per individual.
Here’s a breakdown of the fasting timeline:
4-8 Hours
- Blood sugar drops: The body begins using stored glycogen as blood sugar levels decline.
- Insulin production stops: Insulin levels decrease, signaling the body to switch from glucose to fat as an energy source.
12 Hours
- Digestive system is at rest: The body shifts energy from digestion to cellular repair and maintenance.
- Body begins healing process: Cellular repair mechanisms like DNA repair and autophagy start activating.
- Glucagon balances blood sugar: Glucagon signals the liver to release glucose, maintaining stable blood sugar levels.
- HGH increases: Human Growth Hormone rises to support metabolism, fat burning, and muscle preservation.
16 Hours
- The body starts ramping up fat burning: Glycogen stores are depleted, and the body increases fat oxidation for energy.
18-20 Hours
- Autophagy begins: Damaged and dysfunctional cellular components are broken down and recycled.
- HGH starts to skyrocket: Growth hormone levels increase significantly, aiding tissue repair and fat metabolism.
- Ketones begin to be produced: The liver converts fat into ketones as an alternative energy source for the brain and body.
36 Hours
- Autophagy increases by 300%: The rate of cellular cleanup and repair processes ramps up, removing damaged cells and proteins.
Author’s note: While autophagy does increase significantly with prolonged fasting, a 300% increase isn’t 100% confirmed in human studies and could vary widely from person to person.
48 Hours
- HGH increases by 500%: Growth hormone peaks, enhancing muscle preservation and fat burning.
- Inflammatory response is reduced: Fasting decreases pro-inflammatory markers, promoting tissue healing.
Author’s Note: HGH can increase substantially during fasting due to reduced insulin and increased fat metabolism, but the exact percentage varies by person and may not consistently reach 500%.
54 Hours
- Insulin sensitivity increases: Cells become more responsive to insulin, improving blood sugar regulation.
- Glycogen stores are drained: Stored carbohydrates in the liver and muscles are nearly depleted, forcing reliance on fat and ketones.
72 Hours
- Autophagy peaks: Cellular repair processes are at their maximum, rejuvenating cells and supporting longevity.
Pro Tip: When fasting, you can drink water, plain tea, or black coffee as these do not break the fast. Also, I like to use small amounts of Himalayan salt and apple cider vinegar during extended fasts.
If you don’t think you can handle a full fast, a Fasting Mimicking Diet (e.g., 300 to 1100 calories per day of broths, soups, juices, nut, herbal teas) could give similar results.
A Fasting Mimicking Diet is designed to trick your body into thinking it’s fasting while still receiving minimal nutrition, promoting autophagy, IGF-1 reduction, and all the other benefits you’d typically get through an extended fasting period.
The diet has even been shown to reduce biological age.
A sample day using Fasting Mimicking would look something like this:
Breakfast:
- 1 cup green tea (unsweetened)
- 1 small handful of nuts (e.g., macadamia, almonds)
Lunch:
- 1 cup of vegetable soup or broth (add olive oil for calories)
- 1 serving of roasted non-starchy vegetables (e.g., asparagus, zucchini, mushrooms) with 1 teaspoon olive oil
Afternoon Snack:
- 1 small handful of seeds (pumpkin or chia seeds)
Dinner:
- 1.5 cups of vegetable broth or soup (again, low-sodium, with olive oil)
- 1 serving of lightly steamed vegetables (e.g., spinach, cauliflower, or Brussels sprouts)
Typically, you’d follow this plan for up to 5 consecutive days once a month.
Author’s note: There are a few companies out there that offer pre-packaged fasting-mimicking meals that take the guesswork out of it (e.g., Prolon)
To sum things up:
Insulin resistance places you at a higher risk for:
- Heart disease
- Type II diabetes
- Hypertension
- Alzheimer’s disease
- Majority of cancers
- All-cause mortality
Insulin resistance can be prevented or reversed by:
- Fasting
- Lowering carbs
- Regular activity (walking)
- Lifting weights
- Losing weight
- Reducing processed foods
- Eliminating seed oils
Reversing your insulin resistance will result in:
- Improved energy
- Less cravings for junk food
- Better skin
- Improved physique
- Enhanced hormonal balance
- Better sleep
- Stronger immune system
- Improved mental health
- Better sexual performance
- Longer lifespan
Final Thoughts
Millions of people today suffer from common issues whose root causes are understudied, overlooked, or dismissed by the mainstream.
These include silent killers like insulin resistance, diabetes, and cardiovascular disease.
But others include low self-esteem, depression, obesity, low testosterone, and porn addiction.
Through the convenience of modern society, powered by fiat currency, we’ve built a world of abundance—but often at the expense of our health and freedom, trading vitality and longevity for convenience and lower costs.
Yet, there is hope.
By reading this series, you’ve taken the first step toward change.
The next step is taking action.
Whether you’re battling insulin resistance, type II diabetes, or simply looking to lose 20-30 pounds and reclaim your health, these conditions can be reversed, medications reduced, and your life transformed.
The rest is in your hands.
_______
If you like The Unconquered Mind, sign up for our email list and we’ll send you new posts when they come out.
If you liked this post, these are for you too:
Invisible Economics & The Theory of the Future
Human Action, Alien Evolution, & Predictive Irrationality
Voodoo Math, Alien Economics & LTV
The Rise & Fall of the Modern Nerd
Sources
The facts and opinions in this 2-part series are based on extensive research encompassing hundreds of hours of analyzing scientific studies and expert opinions. It also includes a combination of my own personal experiences and observations, and reflects insights from deep thinkers I know and respect, with whom I’ve had many in-depth discussions on these topics over the past few months.
- Imperatore, G., Boyle, J. P., & Thompson, T. J. (2023). Projections of type 1 and type 2 diabetes burden in the United States: 2020-2060. Diabetes Care, 46(2), 313-326. https://diabetesjournals.org/care/article/46/2/313/148151/Projections-of-Type-1-and-Type-2-Diabetes-Burden
- Longo, V. D., & Panda, S. (2014). Stem cell activation by fasting. Cell Stem Cell, 14(6), 813-819. https://www.cell.com/cell-stem-cell/fulltext/S1934-5909(14)00151-9
- Brandhorst, S., Choi, I. Y., Wei, M., & Longo, V. D. (2016). Cancer therapy and fasting. Frontiers in Oncology, 6, Article 242. https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2016.00242/full
- Di Biase, S., Lee, C., Brandhorst, S., et al. (2022). Fasting-mimicking diet is safe and reshapes immunity in cancer patients. Cancer Discovery, 12(1), 90-105. https://aacrjournals.org/cancerdiscovery/article/12/1/90/675618/Fasting-Mimicking-Diet-Is-Safe-and-Reshapes
- Keynes, J. M. (1936). The general theory of employment, interest, and money. Macmillan. https://amzn.to/3UYZCEr
- Keynes, J. M. (1930). A treatise on money (Vol. 1 & 2). Macmillan. https://amzn.to/3UZbwOo
- de la Monte, S. M. (2022). Insulin resistance and Alzheimer’s disease. Alzheimer’s Research & Therapy, 14(1), Article 12. https://alzres.biomedcentral.com/articles/10.1186/s13195-022-00996-8
- Samuel, V. T., & Shulman, G. I. (2018). Mechanisms for insulin resistance. MDPI Journal of Molecular Sciences, 23(5), Article 2687. https://www.mdpi.com/1422-0067/23/5/2687
- Lal, R., Reicosky, D. C., & Hanson, J. D. (2007). Evolution of the plow over 10,000 years and the rationale for no-till farming. Soil and Tillage Research, 93(1), 1-12. https://doi.org/10.1016/j.still.2006.11.004
- Perry, G., Dominy, N., Claw, K. et al. Diet and the evolution of human amylase gene copy number variation. Nat Genet 39, 1256–1260 (2007). https://doi.org/10.1038/ng2123
- Price, W. A. (2010). Nutrition and physical degeneration: A comparison of primitive and modern diets and their effects. Price-Pottenger Nutrition Foundation. https://amzn.to/4fqZGF3
- Barzun, J. (2000). The dawn of decadence: A portrait of western cultural endings. Harper Perennial Modern Classics. https://amzn.to/3AXK4d2
- Huxley, A. (1923, May). Pleasures. Vanity Fair. https://archive.vanityfair.com/article/1923/5/pleasures
- Chun, O. K., Floegel, A., Chung, S. J., Chung, C. E., Song, W. O., Koo, S. I., & Kim, D. O. (2007). Estimation of antioxidant intakes from diet and supplements in U.S. adults. Journal of Nutrition, 137(12), 3244-3252. https://www.ars.usda.gov/ARSUserFiles/50600000/Products-Reprints/2007/1403.pdf
- Hoppe, H. H. (2001). Democracy: The God that failed: The economics and politics of monarchy, democracy, and natural order. Transaction Publishers. https://amzn.to/4fT42EP
- Ammous, S. (2018). The Bitcoin standard: The decentralized alternative to central banking. Wiley. https://amzn.to/3V0xBfL
- Deaton, A. (2017). Income inequality: Historical and theoretical perspectives. In The Oxford Research Encyclopedia of Economics and Finance. Oxford University Press. https://doi.org/10.1093/acrefore/9780190277734.013.908
- United States Department of Agriculture. (2024). Oilseeds: World markets and trade. Foreign Agricultural Service. https://apps.fas.usda.gov/psdonline/circulars/oilseeds.pdf
- Mises, L. v. (1949). Human action: A treatise on economics. Yale University Press. https://amzn.to/4eJvT9o
- Mises, L. v. (1912). The theory of money and credit. Ludwig von Mises Institute. https://amzn.to/3CAGwOx
- Mises, L. v. (1927). Liberalism: The classical tradition. Liberty Fund. https://amzn.to/3UWsRri
- Menger, C. (1871). Principles of economics (Grundsätze der Volkswirtschaftslehre). Ludwig von Mises Institute. https://amzn.to/3OhPliF
- Menger, C. (1892). On the origins of money. Economic Journal, 2(6), 239-255. https://amzn.to/3ZcR1jW
- Yandle, B., & Smith, A. (2014). Bootleggers and Baptists: How economic forces and moral persuasion interact to shape regulatory politics. Cato Institute. https://amzn.to/4hTpQC3
- Feldstein, M. S. (1985). Domestic saving and international capital movements in the long run and the short run (Working Paper No. 85). International Economics Section, Princeton University. https://ies.princeton.edu/pdf/E85.pdf
- Smith, A. (1981). An inquiry into the nature and causes of the wealth of nations (R. H. Campbell & A. S. Skinner, Eds.). University of Chicago Press. https://amzn.to/3Z0aeE0
- Nutrition Coalition. (2024). Americans follow the guidelines, but their health has not improved.
- Statista. (2024). Various statistics and reports on global trends in health, agriculture, and economics.
- U.S. Department of the Treasury. (2024). National debt: America’s finance guide. Fiscal Data https://fiscaldata.treasury.gov/americas-finance-guide/national-debt/
- Centers for Disease Control and Prevention. (2024). CDC adult obesity facts. https://www.cdc.gov/media/releases/2024/p0912-adult-obesity.html
- Centers for Disease Control and Prevention. (2024). CDC data brief on health statistics. https://www.cdc.gov/nchs/products/databriefs/db508.htm
- Centers for Disease Control and Prevention. (2024). CDC diabetes statistics report. https://www.cdc.gov/diabetes/data/statistics/statistics-report.html
- Centers for Disease Control and Prevention. (2024). CDC childhood obesity facts. https://www.cdc.gov/obesity/childhood-obesity-facts/childhood-obesity-facts.html
- Centers for Disease Control and Prevention. (2024). CDC diabetes data and research. https://www.cdc.gov/diabetes/php/data-research/index.html

